According to the American Psychiatric Association, insomnia is the most common sleep disorder. Difficulty falling and staying asleep are prominent symptoms of insomnia, and prolonged sleeplessness impacts sufferers’ mental and physical health.
Luckily, insomnia is highly treatable. Recent research shows 75 percent of people that experience short-term insomnia return to healthy sleep patterns, never developing chronic symptoms. Those who experience chronic insomnia manage their sleep problems with a few simple lifestyle changes.
Let’s dive deeper into the common causes, different types, and suggested treatments for insomnia.
What Is Insomnia?
As mentioned above, insomnia is a sleep disorder that makes sleep onset (falling asleep) and maintenance (staying asleep) troublesome. People with insomnia also report feeling tired after a full night’s rest and waking up too early without falling back to sleep.
There are two types of insomnia: primary and secondary. Primary insomnia is unrelated to other health conditions and is often the result of a compromised sleeping environment, traumatic event, or stress.
Secondary insomnia is always attributable to an underlying health condition. This may consist of mental or physical health problems and unique sleep disorders, such as sleep apnea. Secondary insomnia can also be a side effect of prescription medication. The two types of insomnia are further characterized by how long they last.
Length of Insomnia
The terms acute and chronic simply describe how often someone experiences insomnia. Primary and secondary insomnia can be acute or chronic. For instance, you may experience acute primary insomnia, chronic secondary insomnia, or vise versa.
Approximately one in four Americans struggle with acute, or short-term insomnia at some point in their life. It is usually the primary type and caused by stress from a serious life event, such as a death in the family, birth of a child, or career shift. Acute episodes occur three nights or less per week and last anywhere from a few days to three months.
More often than not, short-term cases resolve on their own, but they can lead to unhealthy sleeping habits. If insomnia symptoms begin disrupting your daily activities or last longer than three months, they may be classified as chronic.
Chronic, or long-term insomnia requires the assistance of a sleep specialist. Episodes ensue at least three nights per week and last three months or longer.
According to the American Academy of Sleep Medicine, Verified Source American Academy of Sleep Medicine Society focused on sleep medicine and disorders, and the AASM is who authorizes U.S. sleep medicine facilities. View source chronic insomnia affects nearly 10 percent of the population and is commonly caused by unpredictable work schedules, underlying health issues, or poor sleeping habits.Common Causes of Insomnia
Insomnia is often related to environmental factors, emotional issues, or mental and physical health. Below, we have listed and expanded on these common causes of insomnia.
Poor Sleep Habits
Specific habits interfere with our body’s internal clock or circadian rhythm—a 24-hour biological process that controls our sleep-wake cycle by associating certain cues with sleepiness and alertness.
- Completing brain-stimulating or stressful activities before bed, such as playing video games or dealing with work, school, or finances
- Staring at a television, computer, or phone screen before falling asleep
- Having an irregular sleep schedule without a set sleep and wake time
- Eating a big meal or drinking too much caffeine before bed
- Taking naps longer than 30 minutes and/or napping after 3 p.m.
Stress
Significant life changes cause emotional distress that keeps our brain active during the night. These changes may consist of having a baby, losing a loved one, starting a new job, or dealing with financial instability.
Mental Health Issues
Anxiety disorders, such as post-traumatic stress disorder (PTSD), causes mental hyperarousal or moments of high-alert. People in a constant state of high-alert have trouble falling asleep as well as reaching deep and restorative sleep stages.
Other mental health conditions, like depression, induce negative thoughts, also causing hyperarousal and delayed sleep onset. Enjoying life is difficult without enough sleep which may worsen mental health.
In fact, 40 percent of people with chronic insomnia report mental health problems, specifically anxiety and depression. However, mental health issues and insomnia are symptoms of one another, so their relationship is difficult to recognize. The best solution treats both conditions simultaneously.
Neurological Problems
Neurodevelopmental issues, such as attention deficit hyperactivity disorder (ADHD) and autism spectrum disorder (ASD) induce hyperarousal and are often an underlying cause of insomnia.
Neurodegenerative medical conditions, like Alzheimer’s and dementia, can cause bouts of insomnia as well. Alzheimer’s and dementia severely disrupts our circadian rhythm or internal body clock because confusion accompanies daily cues, hampering the sleep-wake cycle.
Prescribed Medication
If you regularly take medication and are experiencing trouble sleeping, consider checking the adverse effects of your prescription, as insomnia is a common side effect of the following medicines:
- SSRI antidepressants used to treat depression
- Stimulants used to treat ADHD
- Nasal and oral decongestants used to treat allergies
- Corticosteroids used to treat inflammation
- Beta-blockers and ACE inhibitors used to treat high blood pressure
- Statins used to treat high cholesterol
- Theophylline used to treat asthma
- Thyroid hormone replacements
Chronic Pain
Physical pain from arthritis, fibromyalgia, cancer, peripheral neuropathy, and other muscle, joint, or bone pain makes finding comfort difficult. This causes tossing and turning and prolongs falling asleep. A mattress for pain relief may alleviate irritating episodes of insomnia.
Hormonal Imbalance
Cortisol, progesterone, estrogen, testosterone, thyroid, melatonin, and growth hormones affect sleep quality. Fluctuations in just one of these hormones can severely disrupt rest.
Other Sleep Disorders
Believe it or not, other sleep disorders induce insomnia. Sleep apnea and Restless Legs Syndrome are the most common conditions behind insomnia.
Sleep apnea is when a person repeatedly stops and starts breathing throughout the night and wakes to gasp for air. Restless legs syndrome is an uncomfortable sensation in the lower extremities that produces an irresistible urge to jerk the legs. Both sleep disorders frequently wake sleepers throughout the night.
Symptoms of Insomnia
Insomnia has a wide variety of causes, but its effects are consistent. People suffering from insomnia experience any combination of the following symptoms:
- Excessive daytime sleepiness
- Irritability
- Difficulty concentrating or remembering things
- Trouble socializing
- Feelings of depression or anxiety
- Increased errors during school or work
- Lack of coordination
- Worrying about sleep
- Less motivation and energy
- Tension headaches
Insomnia Diagnosis
Insomnia can be the sole cause or simply a symptom of mental and physical health problems. So while the disorder is easily identified, the reason behind it is not. Your healthcare provider will ask about your physical health, emotional state, medical history, and sleep habits. They will also carry out a physical exam, have you complete a questionnaire, recommend a sleep diary, and possibly refer you to a sleep center.
The physical exam will pinpoint or rule out any underlying health conditions while the questionnaire will determine the severity of your insomnia. Identifying the cause of your insomnia will probably require more than one visit. Therefore, your doctor may suggest recording when you fall asleep, how long you sleep, and moments you wake throughout the night in a sleep diary. Tracking your sleep patterns in a diary will help your healthcare provider find the root cause of the disorder.
Sometimes, insomnia sufferers are referred for a sleep study. Participants sleep in a comfortable, hotel-like lab while a medical technician tracks brain wave activity, breathing rate, heartbeat, eye movement, and body movement with diagnostic tools, such as electroencephalography (EEG). This practice assists sleep specialists in analyzing specific sleep patterns and identifying potential solutions.
Insomnia Treatment
Cognitive-behavioral therapy is the most effective treatment for chronic insomnia. During the therapy, people with insomnia learn to control and eliminate sleep-preventing thoughts and actions.
Cognitive Behavioral Therapy
Cognitive-behavioral therapy for insomnia (CBT-I) is administered by a sleep medicine specialist and lasts six to eight weeks. During treatment, sleepers practice the following behavioral techniques:
- Sleepers wear biofeedback devices during nighttime. The device aids specialists in identifying and addressing unhealthy sleep patterns by measuring biological signs of sleep, such as heart rate, breathing, and muscle tension.
- Stimulus control therapy phases out sleep-inhibiting actions while maximizing sleep promoting-practices. Sleepers are advised to avoid naps, strictly use the bedroom for sleep, and set a consistent sleep and wake time.
- Relaxation techniques help sleepers calm their mind and body before bed.
- Sleep restrictions teach sleepers to associate their bedroom with rest by requiring they only lie in bed when they are tired.
- Remaining passively awake eliminates anxiety surrounding bedtime by avoiding any purposeful efforts to fall asleep. In other words, sleepers spend less time thinking about how and when they will fall asleep and more time resting.
Insomnia Prevention
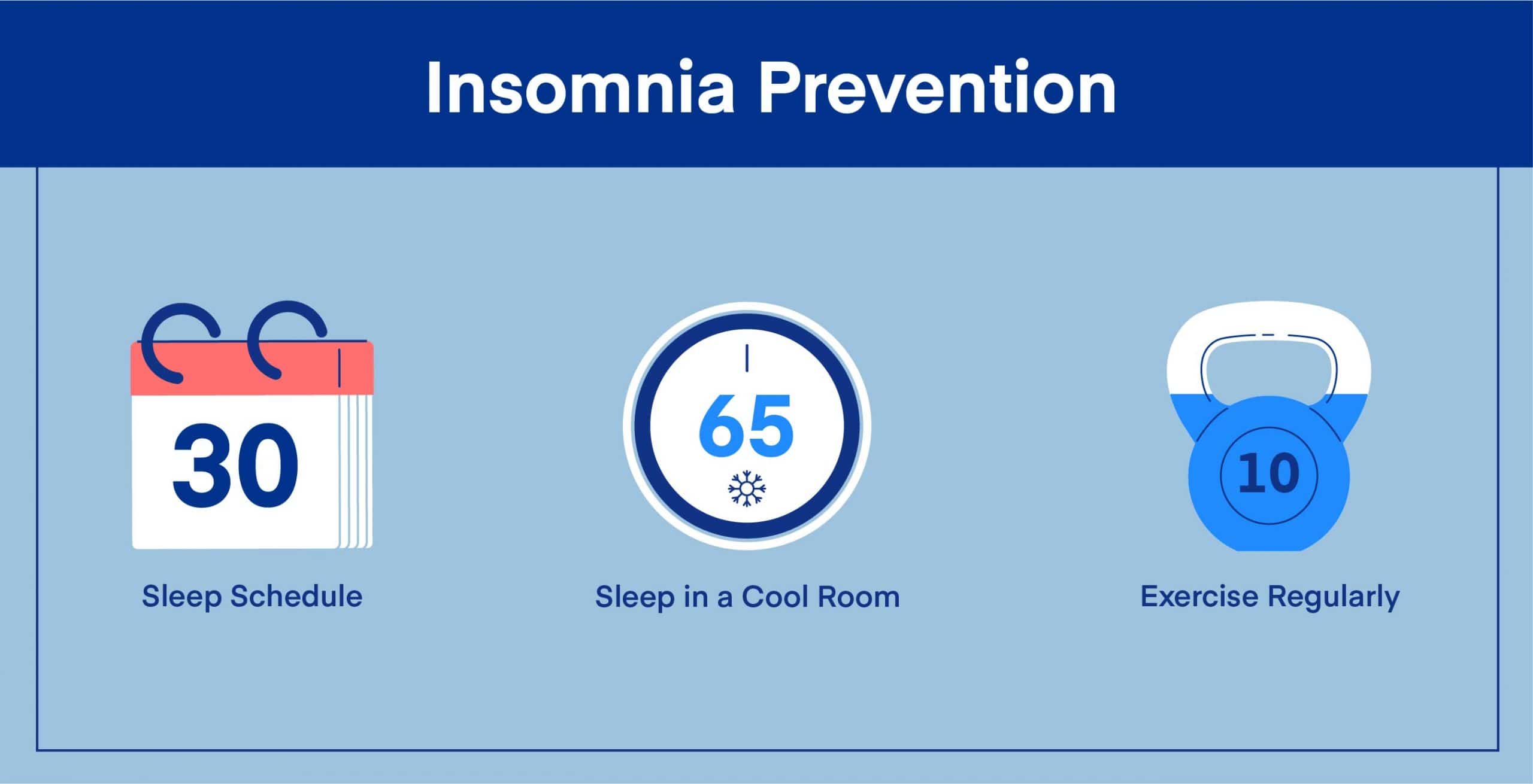
Insomnia sufferers can curb recurring bouts of insomnia by implementing the above techniques into their daily routines. Prevention may look as follows:
- Create a consistent sleep schedule. Maintaining a consistent sleep and wake time will regulate your circadian rhythm. As mentioned above, the circadian rhythm is a biological process that repeats every 24 hours and controls the sleep-wake cycle. If you fall asleep and wake up at a set time, your circadian rhythm will begin promoting sleepiness and alertness at those times each day.
- Establish a bedtime routine. Complete activities you associate with rest before lying down. Activities may consist of reading a book, taking a warm bath, or journaling.
- Sleep in a cool room. Thermoregulation, or fluctuations in body temperature, is an important part of the circadian rhythm and sleep-wake cycle. Drops in body temperature result in sleepiness while increases lead to alertness. However, your core body temperature will drop slower than usual if your bedroom is too hot. This prolongs sleep onset and causes frequent wake time. Keeping your room at 60 to 67 degrees will encourage thermoregulation.
- Avoid bright lights a couple of hours before bed. Light and darkness also affect circadian rhythm. According to the Centers for Disease Control and Prevention, Verified Source Centers for Disease Control and Prevention (CDC) The United States’ health protection agency that defends against dangers to health and safety. View source we are most sensitive to light two hours before bed. Exposing ourselves to bright light within this time frame delays sleepiness. Additional research from Harvard Health Verified Source Harvard Health Blog run by Harvard Medical School offering in-depth guides to better health and articles on medical breakthroughs. View source shows blue light wavelengths from televisions, computers, and phone screens enhance alertness by suppressing melatonin—a naturally produced sleep-promoting hormone.
- Block out distractions from light and noise. People with insomnia struggle to fall asleep and may take longer to reach deep sleep. External stimuli, such as light and noise, make this process even more difficult. Consider shutting out disturbing light with an eye mask and silencing loud noises with earplugs or a white noise machine.
- Exercise regularly. Studies by the National Library of Medicine Verified Source National Library of Medicine (NIH) World’s largest medical library, making biomedical data and information more accessible. View source show 30 minutes of moderate exercise a day improves sleep. Although researchers are unsure why exercise boosts sleep quality, they assume it is because physical activity releases pain, stress, and anxiety-relieving endorphins. These endorphins promote healthier sleep by calming our minds and reducing hyperarousal.
FAQ
Can I take melatonin supplements for insomnia?
The FDA (Food and Drug Administration) does not strictly regulate dietary supplements like melatonin. Therefore, the dosage listed on a label is not always accurate. This is dangerous considering too much melatonin worsens sleep quality and has adverse effects including headache, nausea, joint pain, anxiety, mild tremors, and depression. Unless your doctor has specifically recommended melatonin as a sleep aid, we recommend avoiding the over-the-counter supplement.
Who has a higher risk of insomnia?
People susceptible to health issues or lifestyle behaviors related to insomnia are affected more than others. For instance, insomnia is prevalent in older adults because they are prone to chronic pain, making it difficult to find comfort at night. They are also less physically active during the day, resulting in an overactive mind at night.
Women are another at-risk population because they experience frequent shifts in hormones during their menstrual cycle, menopause, and pregnancy. Although difficult to identify, hormonal imbalance is a common cause of insomnia.
Workers with erratic schedules are also at-risk. An unpredictable work schedule makes creating a bedtime routine or having a set sleep and wake time extremely difficult. Traveling for work intensifies insomnia as well. With traveling, comes jet lag. Jet lag occurs because crossing time zones throws off our circadian rhythm or internal body clock, making regular sleep patterns nearly impossible.
How many hours of sleep do you need per night?
Adults need 7 to 9 hours of sleep Verified Source Centers for Disease Control and Prevention (CDC) The United States’ health protection agency that defends against dangers to health and safety. View source function adequately throughout their day. However, sleeping this amount of time does not ensure quality sleep. Even if we lie in bed for 7 to 9 hours, we may experience frequent waking or never achieve deep sleep. Practicing good sleep hygiene will improve the quality of your rest. This consists of creating a sleep schedule, establishing a relaxing bedtime routine, and making your bedroom cool, dark, and quiet.
What is sleep anxiety?
Sleep anxiety, also referred to as sleep dread, is a type of performance anxiety. Sleep dread is when a person stays up worrying about how and when they will fall asleep. The lack of sleep affects mental and physical health and increases stress. Sleep specialists recommend practicing good sleep hygiene and reminding yourself that experiencing an occasional night of poor rest is perfectly normal.
What is the main cause of insomnia?
Stress is the most common cause of insomnia. Many people spend less time sleeping and more time thinking about tomorrow’s tasks. Combat this anxiety by creating a to-do list before bed. A small study by the American Psychological Association Verified Source American Psychological Association (APA) Collaborative organization for psychologists across the country. View source shows people who write out to-do lists before bed tend to fall asleep faster than those who do not. Researchers believe establishing an at least tentative plan of action for the following day helps sleepers mentally offload their responsibilities.
Conclusion
Restless nights are rampant amongst American adults, with 50 to 70 million reporting a sleep disorder; the most common being insomnia. Although frustrating, poor quality sleep is remediable.
If you find yourself filled with lethargy, irritability, or anxiety from limited rest, there are multiple steps you can take. First, evaluate the reason for your insomnia. Consider your mental and physical health, any distressing turn of events, as well as regularly-taken medication. After determining the potential cause of your poor sleep, begin practicing good lifestyle and sleep habits—go to bed and wake up on time, calm your mind before bed, optimize your sleeping environment, avoid food and caffeine prior to sleep, exercise regularly, and bypass your daily nap.
If renewing your sleep hygiene is ineffective, simply reach out to your doctor. They will get to the bottom of your insomnia and together, you can create a treatment plan fit to meet your unique needs.
About the author
April Mayer has a degree in exercise physiology and is a firm believer in the power of a good night’s sleep. April’s passion lies in helping others lead more productive lives by helping them get sound, restful sleep every night. April primarily writes about foods and vitamins for better sleep and has written several “better sleep guides” covering a wide variety of topics in her time with Early Bird.
View all posts